eLife: Study reveals how Duchenne muscular dystrophy causes heart rhythm problems
Investigadores del CNIC revelan por primera los mecanismos moleculares que subyacen a las arritmias que ocurren en pacientes que padecen “Distrofia Muscular de Duchenne”
Abnormalities in the proteins responsible for transmitting electrical signals in the heart likely cause abnormal heart rhythms in patients with Duchenne muscular dystrophy (DMD), shows a study published in eLife.
The results help explain why as many as 60% of patients with DMD have potentially life-threatening heart rhythm abnormalities. They may also suggest potential treatment strategies for heart problems in people with DMD.
Mutations in a gene that encodes a muscle-protecting protein called dystrophin cause DMD. The condition disproportionately affects males who inherit one copy of the abnormal gene from their mothers. Without functioning dystrophin proteins, patients develop progressive muscle loss. Women who often inherit one functional and one dysfunctional gene copy may have less severe muscle deterioration. But both men and women with DMD are at high risk of life-threatening heart rhythm abnormalities.
“No one knows why patients with DMD develop heart rhythm abnormalities,” explained lead author Eric Jimenez-Vazquez, an assistant research scientist at the Center for Arrhythmia Research at the University of Michigan in Ann Arbor, Michigan USA. “We set out to determine the role of ion channels, which control electrical signals in the heart.”
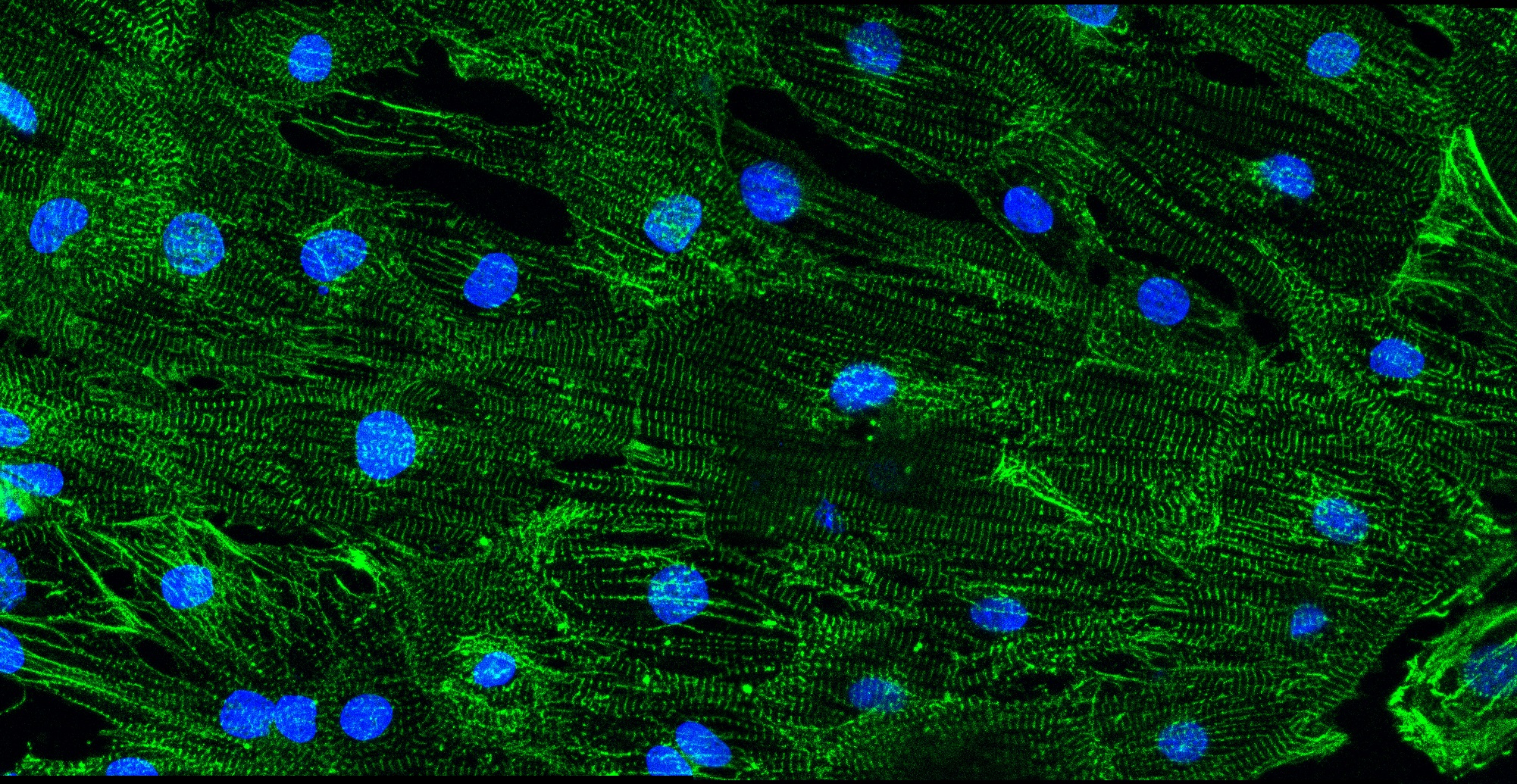
The study was a collaboration of physicians and scientists from four different laboratories in three different countries (the University of Michigan in the USA, the Centro Nacional de Enfermedades Cardiovasculares (CNIC) in Spain, and the Sheba Medical Center and the Technion Institute in Israel). They collected skin biopsies of 3 people with DMD and two healthy volunteers without DMD. Two participants with DMD were males who inherited an abnormal copy of the gene for dystrophin, and one was a woman with one mutant copy and one normal copy of the gene. To determine why the patients developed arrhythmias, in the laboratory, they converted the biopsied cells into stem cells and then coaxed them to become heart muscle cells.
The results help explain why as many as 60% of patients with DMD have potentially life-threatening heart rhythm abnormalities
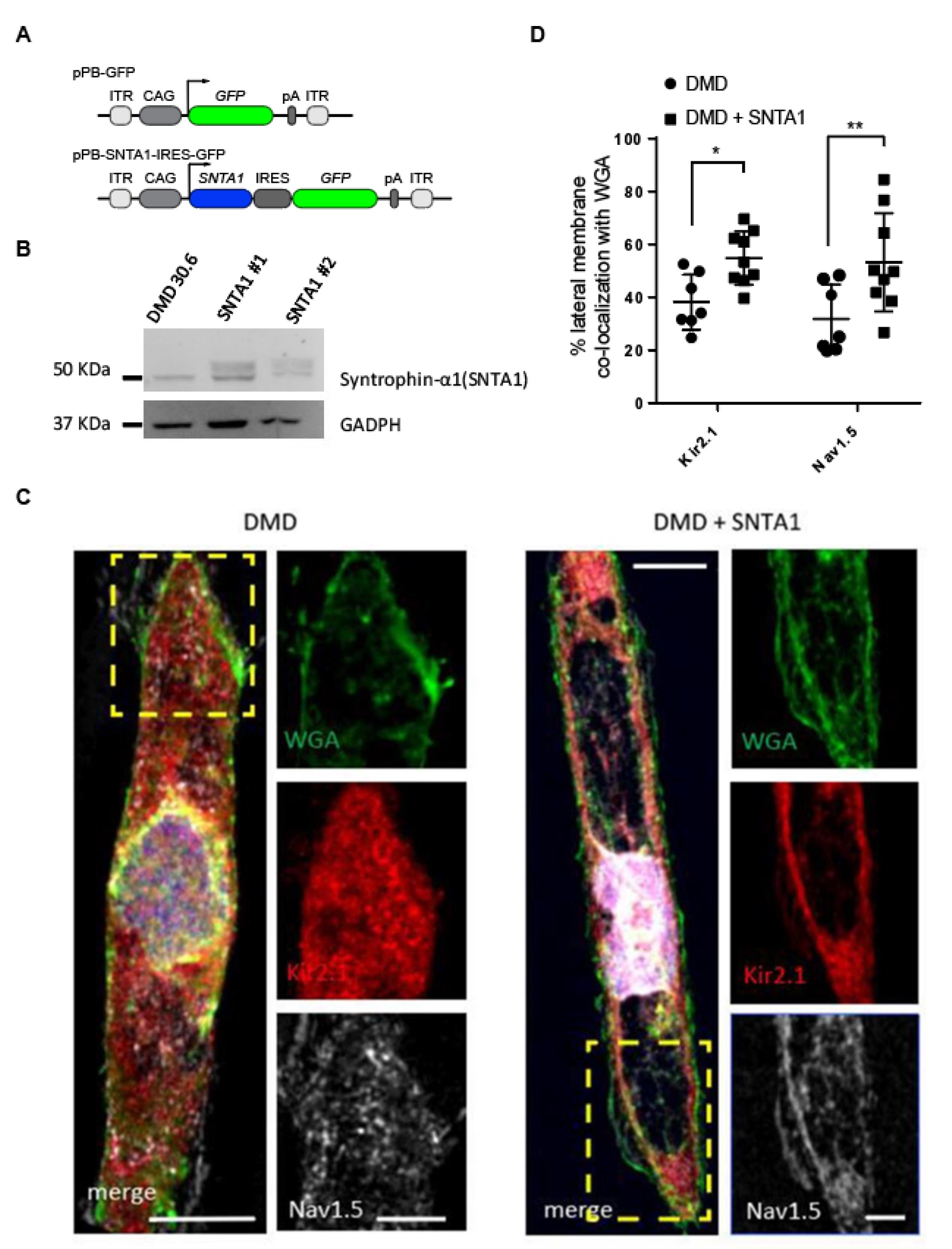
When they measured electrical activity in the newly formed heart cells, they found that cells from people with DMD had slower electrical signals, generated arrhythmias and were less able to contract than cells from people without the condition. Individuals with DMD also had less potassium and sodium ions flowing in their cell membranes, both essential for electrical signalling in the heart. They also found that heart muscle cells grown from the males with DMD had fewer sodium and potassium ion channels, which control the flow of sodium and potassium, than people without the condition.
But adding an essential partner protein of sodium and potassium channels called α1-syntrophin to the cells of one of the males with DMD corrected electrical activity in the cells and prevented abnormal rhythms.
The discoveries may help explain why both males and females with DMD may have life-threatening heart rhythm disturbances. In DMD, males are more often affected but females may be carriers because the dystrophin gene is located on the X chromosome. Since males have one X and one Y chromosome, if they inherit the DMD mutation from their mother´s X chromosome, they do not have a way to make any active dystrophin protein. Thus, they have a high probability of developing the disease. Since females have two X chromosomes, they do not usually have disease symptoms because they can still make dystrophin from their good X chromosome. However, the pattern of distribution of the bad chromosome in the heart cells is random and may determine the severity of their symptoms. This inconsistent pattern may also explain why women with DMD are sometimes as prone to heart rhythms as their male counterparts.
“Our study helps explain why people with DMD develop severe heart rhythm abnormalities and may help scientists develop new treatments for this life-threatening complication,” said senior author José Jalife, Distinguished Senior Investigator at the CNIC and Emeritus Professor of Medicine and Molecular and Integrative Physiology at the University of Michigan.
The study was supported by National Institutes of Health; ‘la Caixa’ Banking Foundation; Fundación La Marató TV3: Ayudas a la investigación en enfermedades raras 2020 (LA MARATO-2020); Instituto de Salud Carlos III/FEDER/FSE- Horizonte 2020 - Programa Marco de Investigación e Innovación - Research and Innovation Framework Programme; and Ministerio de Ciencia e Innovación (MCIN).