CNIC scientists coordinate a European project to develop a biomarker for the early identification of the vascular component in Alzheimer disease
The BioClotAD project, coordinated by CNIC scientist Dr Marta Cortés Canteli, has been selected by the EU Joint Programme – Neurodegenerative Disease Research (JPND)
The BioClotAD project, coordinated by Centro Nacional de Investigaciones Cardiovasculares (CNIC) scientist Dr Marta Cortés Canteli, who is supported by Spain's Miguel Servet Program, has been selected by the JPND transnational call for multinational research on novel imaging and brain stimulation methods and technologies for neurodegenerative diseases. BioClotAD will receive €771,430 over the next 3 years, including €227,480 in direct funding to Dr Cortés Canteli’s group at the CNIC.
The JPND (EU Joint Programme – Neurodegenerative Disease Research) is the largest global research initiative aimed at tackling the challenge of neurodegenerative diseases. The JPND aims to increase coordinated investment between participating countries in research aimed at finding causes, developing cures, and identifying appropriate ways to care for those with neurodegenerative diseases (www.jpnd.eu).
The goal of BioClotAD is to develop a neuroimaging biomarker to detect the procoagulant state in the brains of patients with Alzheimer disease (AD).
The BioClotAD consortium brings together 4 research groups at the forefront of European research in the areas of neuroscience, biochemistry, preclinical imaging, radiochemistry, and translational medicine. As well as the CNIC group, the consortium includes the groups led by Dr Manuel Desco of the Instituto de Investigación Sanitaria del Hospital Gregorio Marañón de Madrid in Madrid (IiSGM); Dr Dag Sehlin of the Public Health and Caring Sciences at the University of Uppsala, Sweden; and Dr Susanne Kossatz of the Klinikum rechts der Isar der Technischen at the University of Munich, Germany.
AD is the most frequent form of dementia and probably also the most devastating in terms of its societal impact. Unfortunately, most treatments for AD have failed, in part due to the multifactorial nature of the disease.
In response to the disappointing results of “one target, one treatment” strategies, current AD research seeks to develop personalized therapies that combine several drugs directed at the multiple mechanisms that contribute to the disease.
However, the success of personalized therapy requires the development of accurate diagnostic tools to monitor the various factors that contribute to AD. One of the promising targets for diagnosis and treatment is a patient’s procoagulant status.
The aim of our project is to design a new non-invasive imaging biomarker to identify the procoagulant state in alzheimer
AD includes a vascular component characterized by severe cerebral hypo-perfusion. Reduced cerebral blood flow is also a feature of mild cognitive impairment and even occurs in cognitively unimpaired individuals at high risk of developing AD. This cerebral hypo-perfusion is in part due to a chronic dysregulation of hemostasis in AD.
Accumulating evidence indicates that AD is characterized by a prothrombotic state. This favors the formation of persistent fibrin clots that contribute to the initiation and progression of the disease.
In experiments with the thrombin inhibitor dabigatran in a mouse model of AD, Dr Cortés Canteli’s group at the CNIC has already shown that long-term anticoagulation blocks fibrin deposition; preserves cognitive function, cerebral blood perfusion, and the function of the blood-brain barrier; and reduces neuroinflammation and amyloid deposition (Journal of the American College of Cardiology).
These results have opened the way to future research into the potential of approved oral anticoagulants for the treatment of AD. However, consistent with the multifactorial nature of the disease, this prothrombotic state is not present in all AD patients. It is therefore important to identify those patients who would benefit from anticoagulant therapy.
“The aim of our project is to design a new non-invasive imaging biomarker to identify the procoagulant state in AD,” said Dr Cortés Canteli.
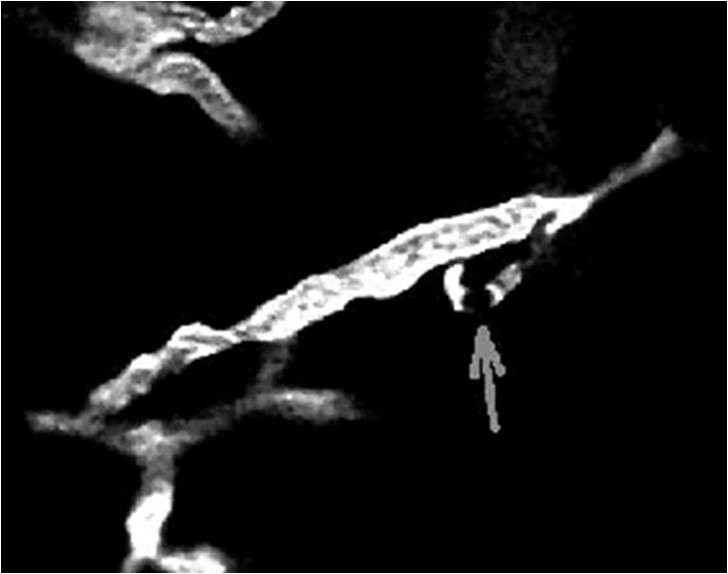
Explaining the strategy, Dr Cortés Canteli continued: “In animal models of Alzheimer disease, we will combine molecular biology approaches with molecular imaging tools to develop a probe to detect fibrin clots both in the cerebral blood vessels and in the brain parenchyma.
Dr. Susanne Kossatz from the University Hospital Klinikum rechts der Isar (TU München) in Munich, Germany, says that she and her team are very excited to be part of this international consortium. Dr. Kossatz’ team will investigate how the novel molecular imaging probes operate on the cellular level. She will conduct tissue-based analyses to confirm the selective and specific nature of the molecular imaging approach of the prothrombotic state under investigation.
Researchers from Uppsala University, led by Dr. Sehlin, will contribute to the project with their expertise in the delivering drugs across the blood-brain barrier, which restricts the passage of molecules between blood and brain. Using a molecular ‘Trojan horse’ strategy, the probe will be modified to interact with receptors in the blood-brain barrier. This will facilitate transport of the probe into the brain parenchyma, where it can find and interact with fibrin clots.
The Uppsala group has previously used a similar approach to transport radiolabeled antibodies into the brain of mice for PET imaging of Alzheimer pathology.
“We see great opportunities in this collaborative project that we believe will open new avenues for Alzheimer diagnosis and therapy”, said Dr. Sehlin.
“BioClotAD”will receive €771,430 over the next three years, including €227,480 in direct funding to Dr Cortés Canteli’s group at the CNIC
This probe will be used to preselect Alzheimer patients with a prothrombotic state for inclusion in clinical trials or for antithrombotic therapy. Crucially, the biomarker will also prevent inappropriate prescription of oral anticoagulants to patients lacking this prothrombotic state.
Although the risk of intracranial hemorrhage with direct oral anticoagulants is low, it is not inexistent. It is therefore important to carefully evaluate each patient’s case in a precise and personalized way. The biomarker developed in this project will play a fundamental role in this process.
According to Dr. Manuel Desco, from the Gregorio Marañón Health Research Institute and head of the CNIC's Advanced Imaging Unit, "The paradigm of personalized and precision Medicine will be applied in numerous pathological processes, undoubtedly including Alzheimer's disease. The so-called molecular imaging can be a tool of extraordinary value in many aspects of the disease, including diagnosis, the selection of effective treatments or the establishment of a precise prognosis. In this line, our group collaborates in the development of new imaging probes that allow characterizing the pathophysiology of the disease in a non-invasive way ".











