The RESILIENCE trial: preventing heart injury caused by anticancer drugs
RESILIENCE is a clinical trial funded by the European Commission (H2020 Programme) that aims to reduce the prevalence of heart failure in cancer survivors
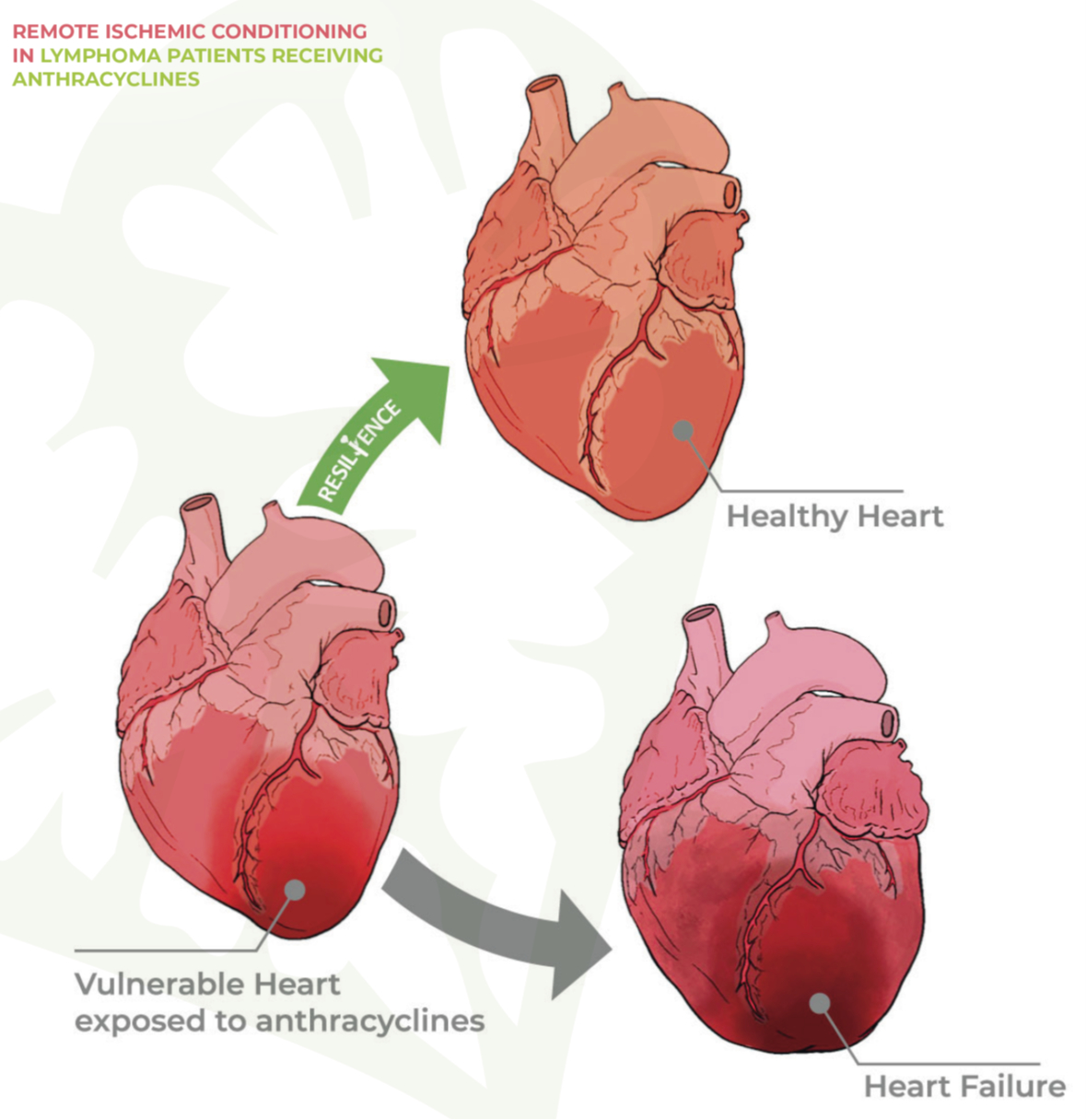
The RESILIENCE clinical trial has been designed to explore the effectiveness and safety of remote ischemic conditioning (RIC) used to prevent the cardiotoxic effects of anthracyline-based chemotherapy in patients with lymphoma. As described in a recent European Journal of Heart Failure editorial this international double-blind clinical trial promises to generate new knowledge and provide possible treatments for this major clinical challenge.
Anthracycline cardiotoxicity continues to be a major concern for patients receiving chemotherapy because of the limited availability of effective protective treatments. Experiments with preclinical models have shown that RIC has cardioprotective effects, paving the way for this innovative clinical trial. RIC consists of repeated brief interruptions of blood flow in a limb, usually an arm; the idea is that this exposure to transient ischemia will protect distant vital organs such as the heart against injury caused by subsequent injurious episodes such as the cytotoxic actions of chemotherapy agents. The RIC´s temporary cessation of blood flow in the arm is achieved with arm cuffs very similar to those used to measure blood pressure, but in RIC the cuff is inflated for a full 5 minutes before being deflated. The process is repeated up to 4 times in each session.
RESILIENCE is financed by the European Commission (H2020 Programme), and its goal is to reduce the prevalence of heart failure in cancer survivors and thus improve their quality of life. The trial is coordinated by the Centro Nacional de Investigaciones Cardiovasculares (CNIC) under the leadership of Dr. Borja Ibáñez, and among the key project partners is the European Society of Cardiology, which will lead one work package and participate in several other activities within the consortium.
The other partners on the project are the Instituto de Investigación Sanitaria Fundación Jiménez Díaz and the Centro de Investigación Biomédica en Red (CIBER) in Spain; the Instituto Português de Oncologia and Hospital da Luz in Portugal; the Centre Henri Bequerel in France; Universitätsklinikum Düsseldorf in Germany; Amsterdam Academic Medical Center in the Netherlands; and Aarhus Universitetshospital in Denmark. The technology partner in the consortium is Philips Healthcare, which coordinates the imaging technology used in RESILIENCE. The trial also enjoys the participation of the Lymphoma Coalition Europe patients’ association. The ESC is an especially important partner as it acts as the nexus for stakeholders from outside the project. The lead ESC scientist on the project is Dr. Teresa López-Fernández, a world authority in the field who directed the ESC 2022 cardio-oncology clinical practice guidelines.
Recent data show that more than 1 in 3 patients receiving anthracyclines develop some form of treatment-induced cardiomyopathy
Cancer patients are a vulnerable population at risk of developing cardiovascular complications. Some of these adverse cardiovascular effects are caused by drugs used to treat cancer. Anthracyclines are highly effective against many types of cancer, including the various forms of lymphoma, breast cancer, leukemia, melanoma, and uterine and gastric cancers. However, these drugs have a potential toxic effect on the heart that can lead to chronic heart failure.
Of the 4 million cancer patients diagnosed in Europe each year, more than 3 million are treated with anthracyclines (alone or in combination with other treatments). Recent data show that more than 1 in 3 patients receiving anthracyclines develop some form of treatment-induced cardiomyopathy. In Europe, an estimated 1 million people have chronic heart failure secondary to chemotherapy-induced cardiomyopathy.
RESILIENCE is led by Dr. Borja Ibáñez, CNIC General Director, a cardiologist at Hospital Universitario Fundación Jiménez Díaz in Madrid, and a group leader in the Spanish cardiovascular research network (CIBERCV). Dr. Ibañez explained that the main goal of RESILIENCE is “to perform a randomized clinical trial testing the cardioprotection provided by remote ischemic conditioning against anthracycline cardiotoxicity.”
Dr. Ibáñez added that there is solid experimental evidence supporting the idea that RIC can significantly reduce the damaging effect of anthracyclines on the myocardium. “The patients included in the trial are those with a high cardiotoxic risk. The trial will also test the ability of new cardiac magnetic resonance (CMR) imaging methods to identify the early signs of the cardiotoxic action of anthracyclines.” The trial will include a total of 608 lymphoma patients. So far, more than 220 participants have been recruited to the trial.
Another unique feature of the RESILIENCE trial is the use of the latest generation CMR technology to investigate the effect of RIC on heart function and composition. Study participants will be randomized to receive weekly RIC or a dummy procedure throughout their chemotherapy treatment. The patients will be examined by multiparametric CMR at three key time points: at the start of the study, halfway chemotherapy (i.e. after the third chemotherapy cycle, intermediate CMR), and two months after the end of the chemotherapy treatment. These CMR scans will monitor changes in heart function, with particular focus on left ventricular ejection fraction (LVEF).
After completion of chemotherapy, the patients will be monitored for possible clinical events over a follow-up period of 24 months or more. The main outcome measure will be the change in LVEF from the beginning of the study. Secondary outcomes include the incidence of cardiotoxicity-related events, identified by specific drops in ejection fraction. LVEF is the most important measure of cardiac function. This parameter, expressed as a percentage, measures the reduction in volume of the left ventricle in systole (contraction) relative to diastole (relaxation). Thus, an LVEF of 50% indicates that the contracting left ventricle reduces its volume by half relative to the relaxed state.
According to Dr. Andrea Moreno-Arciniegas, the cardiologist supervising the CMR studies in RESILIENCE, “the trial will test the predictive capacity of the latest generation CMR technology versus that of established markers such as left ventricular deformation and cardiac injury biomarkers”. RESILIENCE will also validate a new magnetic resonance sequence for ultra-rapid cine acquisition, with the aim of reducing scan times for this vulnerable population.
The RESILIENCE trial represents a significant advance in the development of cardioprotective strategies for cancer patients with a high risk of anthracycline-induced cardiomyopathy. “All the patients included in the trial have some characteristic that places them at high risk of this cardiac complication secondary to cancer chemotherapy,” concluded Dr. Ibáñez.
The RESILIENCE trial is funded by the European Commission (H2020-HEALTH, grant number 945118).